B e f o r e :
NEIL MOODY KC SITTING AS A DEPUTY JUDGE OF THE HIGH COURT
____________________
Between:
| |
MR STUART RUNCIMAN
(on his own behalf and as Executor of the Estate of Susan Alexander Deceased)
|
Claimant
|
| |
- and -
|
|
| |
UNIVERSITY HOSPITAL SOUTHAMPTON
NHS TRUST
|
Defendant
|
____________________
Kate Lumbers (instructed by Thompsons Solicitors LLP) for the Claimant
Matthew Barnes (instructed by DAC Beachcroft LLP) for the Defendant
Hearing dates: 29, 30 April, 2, 3 May 2024
____________________
HTML VERSION OF APPROVED JUDGMENT�
____________________
Crown Copyright ©
This judgment was handed down remotely at 10.30am on 12 July 2024 by circulation to the parties or their representatives by e-mail and by release to the National Archives.
.............................
NEIL MOODY KC (SITTING AS DEPUTY HIGH COURT JUDGE)
NEIL MOODY KC:
Introduction
- This is an action for damages for clinical negligence. The Claimant, Mr Stuart Runciman pursues a claim arising from the death of his wife Mrs Susan Alexander who died at Southampton General Hospital on 4th August 2018 after suffering a cerebral venous sinus thrombosis. The central allegation is that her condition was misdiagnosed as an arterial ischaemic stroke. It is further alleged that this erroneous diagnosis led to Mrs Alexander being given alteplase (thrombolysis), a "clot-buster" drug, instead of heparin, an anticoagulant. The Claimant alleges that, if Mrs Alexander's condition had been correctly diagnosed and properly treated, she would have made a good recovery. The Defendant Trust denies breach of duty. It says that the diagnosis (whilst seen to be incorrect in hindsight) was a reasonable one to make at the time and the treatment was therefore appropriate. The Defendant says further that, even if the correct diagnosis had been made and heparin had been administered instead of alteplase, it would have made no difference to the outcome. Alternatively, the Defendant says that if Mrs Alexander had survived, it would have been with a reduced life expectancy and significant disability.
- Mr Runciman brings this action on behalf of Mrs Alexander's estate under the Law Reform (Miscellaneous Provisions) Act 1934 and for the benefit of her dependants pursuant to the Fatal Accidents Act 1976. The claim is put at £284,643. The Defendant Trust was at all times responsible for the operation of Southampton General Hospital and vicariously liable for the acts and omissions of its clinicians.
Mrs Alexander
- Mrs Alexander was born on 1st April 1959. She married Mr Runciman in 2010. (He said that she changed her name to Alexander in 2013 because of the difficulties some people had with the name Runciman.) She had two sons, Ian Dane and Joe Tubb, and a daughter, Nikki Dane. She was employed by Hampshire County Council as a school escort, taking children with special needs to school.
- Mr Runciman provided a witness statement which gave a moving account of the distressing events that led to his wife's death, the effect they had on him and their wider family. He said that he has "struggled to come to terms with Sue's passing." He works at the hospital as a porter, and he said that he "can't get away from the loss, either at work or at home." Mrs Alexander's son, Ian Dane, provided a witness statement describing their close relationship and the strong family support she provided to him and his siblings. Neither Mr Runciman nor Mr Dane were required to give evidence as their witness statements were agreed.
Cerebral venous sinus thrombosis
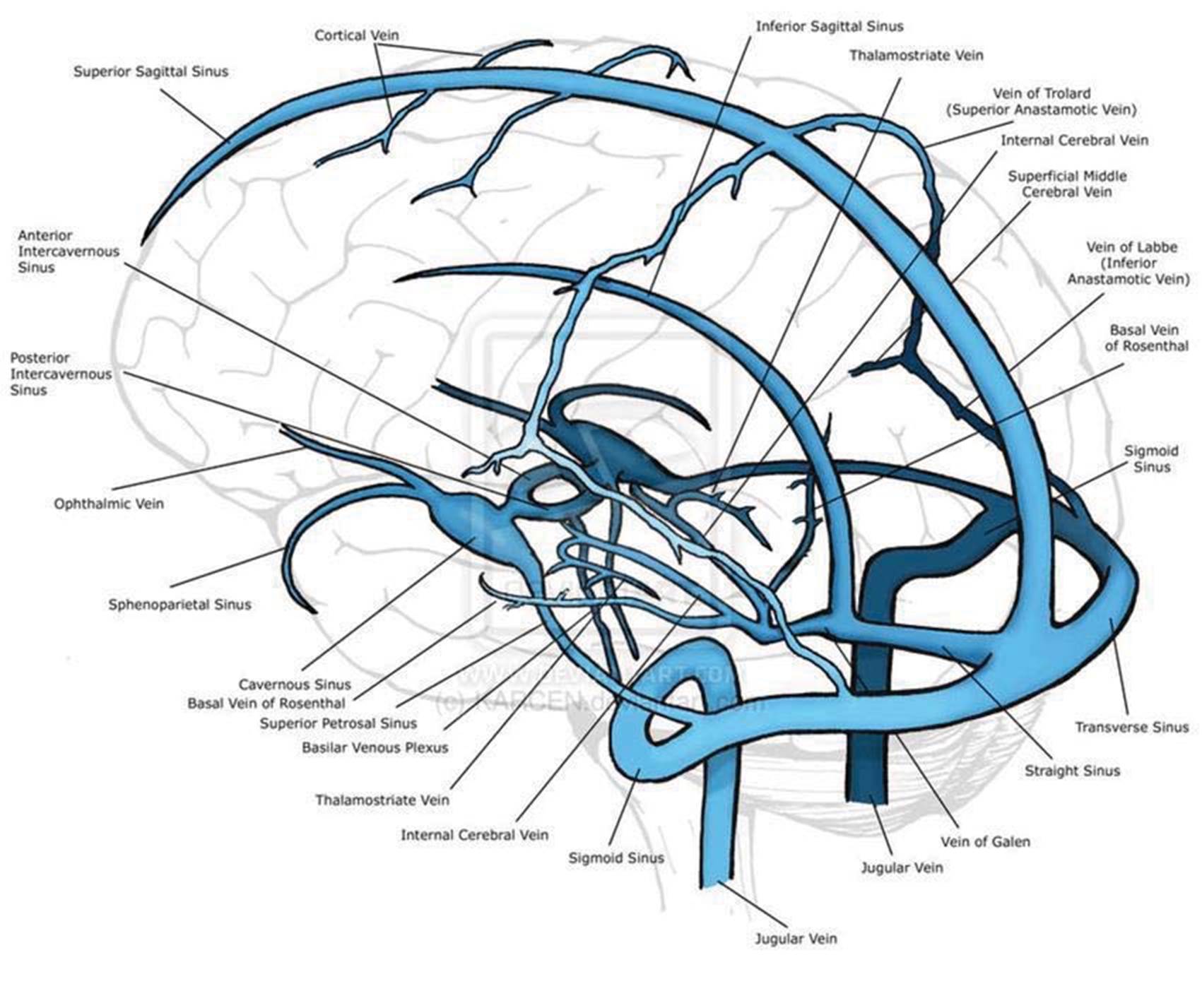
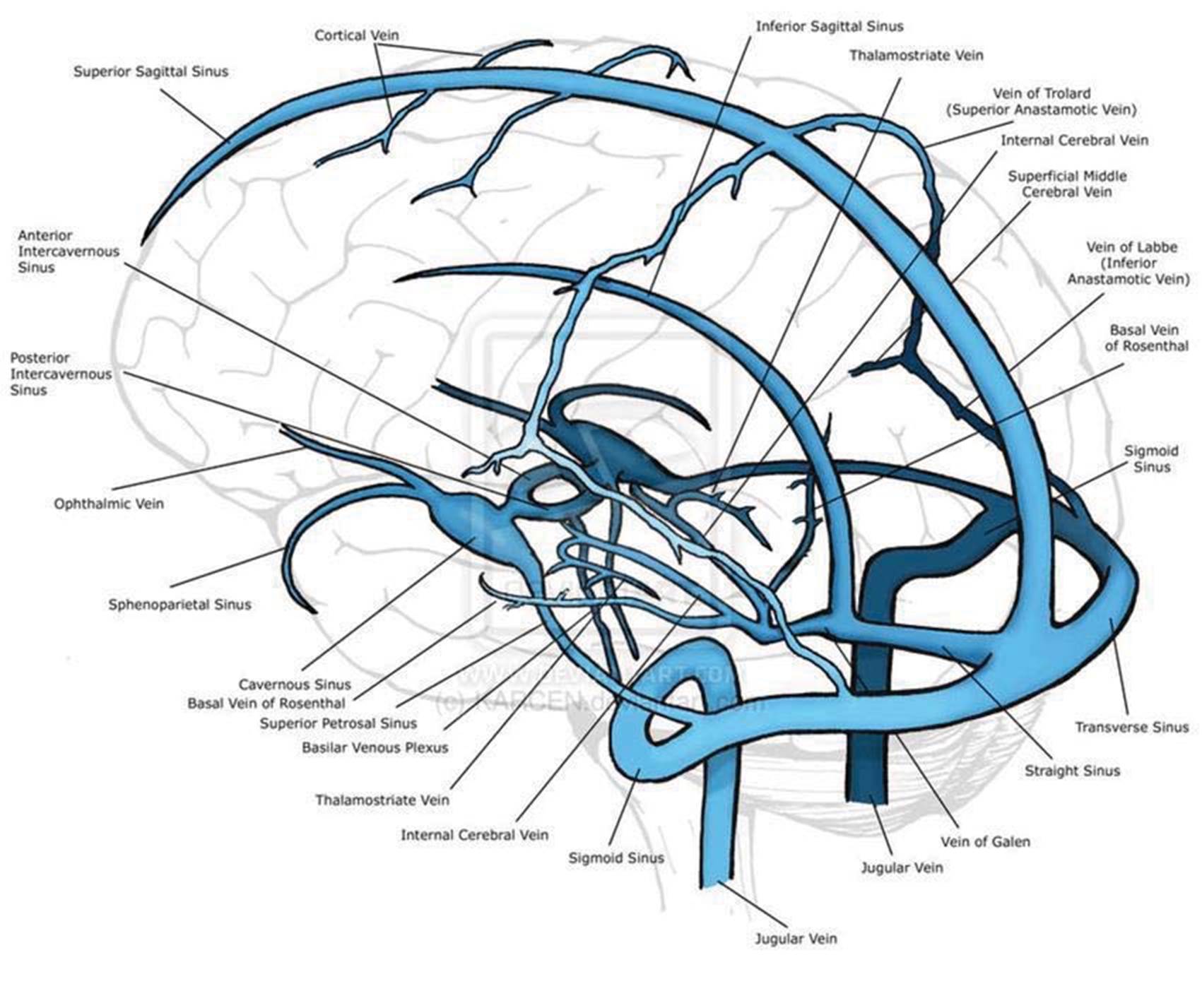
- The central dispute in this case revolves around cerebral venous sinus thrombosis ("CVST" although it was sometimes referred to in evidence as "VST" or "CVT") and arterial ischaemic stroke ("AIS", sometimes referred to in evidence as acute ischaemic stroke). These are both types of strokes. Oxygenated blood is pumped from the heart to the brain at high pressure in the arterial system. It is then returned to the heart via the venous system at lower pressure. This creates a pressure gradient. A cerebral venous sinus thrombosis is caused by a blood clot (thrombus) which occurs in the cerebral venous system. It may restrict flow to a greater or lesser extent, depending on the size of the thrombus. AIS occurs in the arterial system. Most of the features of the cerebral venous sinuses referred to in this judgment are shown in this diagram. The thrombus in question was in the superior sagittal sinus. The thrombus was described in evidence as like a cord or "snake-like".
- The following points were agreed in the expert neurologists' joint statement. CVST is uncommon in clinical practice. It accounts for 0.5% of all stroke patients admitted to hospital. The condition is more common in females than males with a ratio of 3:1. There are myriad causes and presentations. The onset can be acute, subacute or chronic. It most often presents with new headache or as a syndrome of isolated hypertension. Additional manifestations include focal neurological deficits, seizures and/or encephalopathy.
- Dr Durkin, the expert stroke physician called by the Defendant, produced an extract from Neuroanatomy, Superior Sagittal Sinus (Letchuman V, Donohoe C) which states:
"Clinical Significance
Due to its multiple connections including its significant role in draining the cerebral hemispheres… there are multiple complications and pathological processes that can affect the superior sagittal sinus….
First and foremost, the superior sagittal sinus is prone to thrombosis, presenting with various features from headaches, hemiparesis, sixth nerve palsy, papilledema, nausea, and seizures…
Superior sagittal sinus thrombosis is of extreme clinical importance due to the irreversible consequences that can occur secondary to the increased intracranial pressure that is associated with dural vein occlusion….
Heparin is the mainstay of acute treatment…
Identification of this condition can be challenging but in the face of a high index of clinical suspicion computed tomography (CT) venography, magnetic resonance venography or intentional catheter arteriography with attention to the venous phase can be diagnostic.
- A number of medical papers were adduced in evidence. The International Study on Cerebral Venous and Dural Sinuses Thrombosis ("ISCVT") examined 624 cases. Of these 78% occurred in patients younger than 50. Both parties referred to Cerebral venous sinus thrombosis: Etiology, clinical features, and diagnosis, J M Ferro et al., 2021. This noted that the median age of CVST patients was 37 and only 8% were older than 65. Compared with males, females were significantly younger, with a median age for females of 34 and a median age for males of 42.
- The Ferro paper addresses the pathophysiology and explains that there are two processes by which CVST may cause injury: (a) obstruction of the blood drainage resulting in tissue damage and bleeding, and (b) decreased cerebrospinal fluid absorption resulting in raised intracranial pressure. (It has not been suggested that the second mechanism was a feature of Mrs Alexander's condition.) As to the first process, Ferro explains that "obstruction of the venous structures results in increased venous pressure, decreased capillary perfusion pressure, and increased cerebral blood volume." He then explains that this may have one or more of the following consequences: (a) the increase in venous and capillary pressure may result in disruption of the blood brain barrier, causing oedema and leakage of blood plasma; (b) the increases in venous and capillary pressure may result in venous and capillary rupture and so haemorrhage; and (c) the increase in venous and capillary pressure may alter the pressure gradient between the arteries and veins and so result in impaired perfusion of the brain, and so ischaemia, infarction, and haemorrhage.
It was common ground that diagnosing and treating any stroke is urgent. It was also common ground that CVST cannot usually be diagnosed on the basis of a plain CT scan; a CT Venogram ("CTV") is required. It was agreed that the appropriate treatment for CVST would be heparin, an anticoagulant. Heparin works, not by dissolving the clot, but by preventing the propagation of the thrombus and allowing the body's own mechanisms to "recanalise" the veins.
- As for arterial ischaemic stroke, it was agreed that (a) treatment with thrombolysis improves outcomes; (b) treatment with thrombolysis must take place within a window of 4.5 hours from the acute onset of the focal neurological symptoms; and (c) within that 4.5 hour period, treatment should be administered as soon as possible. This was encapsulated in the vivid phrase "time is brain". Indeed, the time from "door to needle" in individual hospitals is subject to national monitoring. Thombolysis is the process of giving the drug alteplase. The drug is also referred to as recombinant tissue plasminogen activator or "rt-PA" and sometimes described as a "clot buster" as it works by dissolving the clot.
The relevant history
- The history as set out in this section is common ground save where I indicate otherwise. It is largely drawn from the medical notes. The notes were relied upon by both parties as evidencing Mrs Alexander's symptoms and signs and the decisions made by the treating clinicians. I accept them as evidence of such.
- On 11th July 2018, Mrs Alexander developed a bad headache. Early in the morning on 13th July Mr Runciman was sufficiently concerned that he telephoned the out-of-hours GP, who sent an ambulance. On examination by the ambulance crew, Mrs Alexander was pale and clammy. She was FAST[1] negative. It was recorded that she had been complaining of diarrhoea and vomiting since 2am and that she had had a headache for two days which came on gradually and was across her forehead. No neurological deficits were present. She was lightheaded on standing. She reported feeling more lethargic the previous day; she had wanted to sleep but had to work. The ambulance crew gave advice and declined to take her to hospital. The working diagnosis was recorded as "viral".
- During the evening on the following day, 14th July, Mr Runciman said that he was so worried that he again rang for an ambulance. Mrs Alexander was complaining of the same symptoms with bilateral lateral chest pain. The history of diarrhoea and vomiting was recorded. It was noted that Mrs Alexander had a headache which had gradually worsened over the last four days. On examination she was alert with a Glasgow Coma Score ("GCS") of 15/15 and no focal neurology. At 22.44 the FAST assessment was recorded as "No Facial Weakness, No Arm/Leg Drift, Speech Normal." The paramedic recorded: "Impression (1) viral gastroenteritis (2) MSK [musculoskeletal] chest pain due to vomiting." He declined to take her to hospital and gave her an Ondansetron anti-nausea injection.
- On 15th July, a Sunday, Mrs Alexander woke as normal but at 08.30 she developed sudden onset speech disturbance and right sided weakness. Mr Runciman called an ambulance at 09.10 and paramedics attended at 09.17. It was recorded that the patient had started to develop problems with her speech and then developed right arm and right leg weakness. The FAST assessment showed "no facial weakness; arm/leg drift; [affected side] right side; speech impaired." On examination it was recorded that the patient was "alert and orientated", with a GCS of 15. There was "slurred speech and profound right sided arm and leg weakness" upon the arrival of the rapid response vehicle, but this "seemed to have improved to some degree since initial assessment". There was no facial palsy. When reassessed, the patient was "globally weak throughout but focally weaker on the right arm and leg". Speech was "slow and deliberate". The impression was that the patient was "struggling to form words". It was recorded: "5/7 pmh [past medical history] frontal headache. Constant and 8/10". There had been diarrhoea and vomiting for 48 hours. The plan was to pre-alert the stroke team and convey Mrs Alexander to hospital without delay. It was then recorded "[Patient] remains as described above until arrival and handover at ED but thereafter does not seem able to speak at all."
- Mrs Alexander was taken to Southampton General Hospital. The on-call specialist neurology registrar was Dr Vijay Nar. The on-call consultant was Dr Rhiannon Morris. They both gave evidence at the trial and I address their evidence below.
- Mrs Alexander was assessed in the stroke unit by Dr Nar. He said, and I accept, that he did not see the ambulance service notes at the time, but he received a verbal handover. His own notes record:
4/7 ago front HA [headache] Gradual onset. Pressure-type. Only minimal relief with paracetamol and ibuprofen. No deficits. 2/7 diarrhoea and vomiting. Called paramedics last night. Ondanestron given. No focal neurological deficit noted. Woke up this morning as normal but still nauseous according to husband. @ 08.30 sudden onset of speech disturbance & RSW [right sided weakness]. Paramedic arrived noted dense RSW. Ambulance arrived & mild improvement but still weak and speech still not normal…
- He examined Mrs Alexander and his notes record:
Pupils equal and reactive. Difficult to assess VF [visual field] but appears intact. No gaze preference. Full EOM [extraocular movement]. No facial droop. ?Subtle R lower-lip. RUL [right upper limb]: flacid weakness. Brisk reflexes. RLL [right lower limb]: some antigravity but collapses back to bed within 1-2 secs. ? and brisk reflexes. Extensor plantar R. Withdrawal. LUL [left upper limb] strong. LLL [left lower limb]: strong.
Unable to move objects. Able to answer Yes/No to simple questions. Unable to tell me day/date/time/month/year. Follows 1 step commands only.
- Dr Nar said in his witness statement and in evidence that headache was not one of Mrs Alexander's primary complaints at presentation. He said that it was "verbally handed over" by the ambulance service that she had a headache.
- In his witness statement he said that once his examination was concluded Mrs Alexander was "rushed" into the CT scanner. He said that before she underwent the CT scan he carried out fundoscopy in order to check for raised intracranial pressure. The result was normal. This was not recorded in his notes, but – for reasons which I explain below at paragraph 43 – I accept this evidence. Fundoscopy allows a full examination of the internal structures of the eye. It may demonstrate papilloedema (swelling of the optic disc due to raised intracranial pressure). Raised intracranial pressure is an important indicator of CVST.
- At 10.12 a head CT scan was carried out. The request form was completed by Dr Nar and stated: "Clinical history – 2 day history D+V, today 08:30 developed right sided weakness and slurred speech, ?acute stroke." At 10.32 the CT head was provisionally reported by Dr C Brook, radiology specialist registrar:
Unenhanced CT brain. No acute intracranial haemorrhage. No extra axial collections. No mass effect or loss of grey-white matter differentiation to suggest acute ischaemia. The ventricles are within normal limits. The basal cisterns are patent. No skull abnormality is seen. The mastoid air cells and paranasal sinuses are clear. Conclusion – No acute intracranial abnormality"
- The parties' expert neuroradiologists agreed that this scan was within normal limits save that there was abnormal high density in the superior sagittal sinus. With hindsight it can be seen that this was clearly indicative of CVST. This was not reported at the time, but the Claimant's expert neuroradiologist said that the signs were subtle and he made no criticism of this.
- Dr Nar said, and I accept, that he discussed the CT scan with the radiologists at the time. His witness statement did not refer specifically to discussing CVST but he said in evidence that it was discussed and it is supported by his own note of the CT head which records: "Falx calcification. No obvious infarct or haemorrage. No dense vessel. No hyperdensity to suggest VST." I find that this shows that CVST was considered by Dr Nar at the time.
- Dr Nar discussed Mrs Alexander's case with Dr Rhiannon Morris, the on-call consultant. This was necessary not least because, at Southampton, the decision to administer thrombolysis had to be made by a consultant. (This is not the case in all hospitals.) I address the evidence as to their discussions in more detail below.
- Dr Nar's diagnosis and management plan stated:
Imp[ression] L MCA [middle cerebral artery] infarct ?aetiology
1. Admit to HASU [hyper acute stroke unit]
2. tPA [alteplase] given after explanation of risks
- At 10.40 Mrs Alexander scored 11 on the NIH Stroke Scale. According to Dr Durkin, this indicated a moderately severe stroke. From 10.43 Mrs Alexander was treated for a presumed left middle cerebral artery ischaemic infarct by intravenous infusion of alteplase. The first 10% was given as a bolus dose, and 90% infused over the next hour. I find therefore that the "door to needle" time (ie the time taken from arrival in the unit to thrombolysis) in Mrs Alexander's case was 43 minutes. (The notes show that she was first seen by a stroke nurse at 10am.)
- Thereafter Mrs Alexander's condition deteriorated and Dr Nar was called to see her. Her GCS dropped to 8. A repeat CT head was undertaken at 12.09. The clinical history given to the radiologist stated: "thrombolysed for presumed left mca infarct at 10.43, worsened GCS since, not obeying commands, ?ICH [intracerebral haemorrhage]". The report at 12.30 stated:
There are bilateral foci of acute haemorrhage in the parasagittal white matter of the right and left superior parietal lobes. No definite associated loss of grey-white matter differentiation to suggest acute ischaemia… Minor surrounding sulcal effacement but no gross mass effect is present. The lateral ventricles are not effaced.
No significant hyper density within the venous sinus is seen to suggest thrombus but the bilateral nature of the haemorrhagic foci would raise sinus venous thrombosis as underlying diagnosis…
Conclusion: Bilateral hemorrhagic foci in the apex of the parietal lobes. The possibility of an SVT has been raised with the team. CT venogram advised.
- The CT scan report thus made two important points. First, there was a new haemorrhage and secondly, CVST was clearly indicated. As with the earlier CT head, the scan was provisionally reported by the neuroradiology registrar on call and the report later confirmed by the consultant neuroradiologist.
- Dr Nar said that his initial diagnosis had been of a left cerebral hemisphere stroke but the location of the bleeding did not fit with this. It thus raised the suspicion that Mrs Alexander had suffered a CVST. A CTV was undertaken almost immediately after the CT report at 12:32. The clinical history given to the radiologists stated:
Admitted with RSW [right sided weakness] and speech disturbance, thrombolysed as first differential thought to be ischaemic stroke, post-thrombolysis more agitated, rescan shows bi-parietal haemorrhage ? underlying VST.
- The CTV was reported at 13:24 and stated:
There is a long segment filling defect within the superior sagittal sinus likely in keeping with venous sinus thrombosis. Arachnoid granulations are seen within the transverse sinuses but no definite thrombus is identified here. …PROVISIONAL CONCLUSION: Probable superior sagittal sinus thrombosis.
- The severity of the thrombus at this stage is an important feature of the parties' cases on causation, and I return to this below.
- At 13.40 Mrs Alexander's GCS was 8. She was admitted to Neuro-ITU. A further CT head was undertaken two days later at 10.25 on 17th July. The conclusion was:
The left parietal haemorrhage has increased in size and now measures 52 mm in depth with increased mass effect. A neurosurgical opinion is recommended.
The right parietal haemorrhage has decreased in size, and has extended into the ventricular system and corpus callosum.
- There were clinical discussions with neurosurgical and interventional radiology teams, but no active management was planned. Heparin, despite being the preferred treatment for CVST, was not given at this stage. This is because, as an anticoagulant, there were concerns that it could exacerbate the haemorrhage. No criticism is made of this decision. A further CT head and CTV was undertaken on 19th July. The report stated:
As previously, there is filling defect in the anterior and middle portions of the superior sagittal sinus, with mild expansion of the sinus. There is now more confluent filling defect with expansion of the posterior part of the superior sagittal sinus, although there was clot here previously and the change in appearances may relate to maturation of the clot. The filling defect extends just into the proximal portion of both transverse sinuses. As before, clot is seen within the left sigmoid sinus, propagating into jugular bulb at the lowest aspect of the imaged volume. Focal filling defects in both distal transverse sinuses, larger on the left, at the junction of the vein of Labbe, are unchanged and probably represent arachnoid granulations.
1. No increase in the volume of intracranial haemorrhage; maturation of the biparietal venous infarcts with increase in associated oedema
2. Venous sinus thrombosis throughout the superior sagittal sinus, extending into the proximal aspect of both transverse sinuses, with further thrombus in the left sigmoid sinus. There is probably not extension of clot but change in appearances of the posterior superior sagittal sinus probably represents maturation.
3. Signs of raised intracranial pressure.
4. New right frontal subcortical small hypodensity may represent further venous hypertension/infarct.
- Heparin was commenced on 19th July. A CT Head and CTV were carried out five days later on 24th July. Mrs Alexander had not improved. The scans were sought to "check for evidence of recannulation." The report stated:
The left parietal haematoma has matured, reducing in density with increase in the extent of associated oedema. Right parietal haemorrhage is larger than previously and remains of high density suggesting there has been a further acute bleed. There is now an ovoid haematoma here of approximately 2cm in diameter…
On CTV, filling defects persist through the superior sagittal sinus, into the torcular and within the left sigmoid sinus, extending into the jugular vein. However, the affected sinuses are less expanded, suggesting maturation of the thrombus. The distal right transverse sinus is narrowed, likely reflecting raised intracranial pressure.
Conclusion: no evidence of recanalization of the affected venous sinuses. Maturation of most haemorrhage centred on the parietal lobes bilaterally, with increase in associated oedema, but also evidence of a more recent small haemorrhage in the right parietal lobe.
- On 26 July, after family discussions, Mrs Alexander was extubated, heparin was discontinued and she was moved to the ward for palliative care. She appeared to be somewhat better on 1st, 2nd and 3rd August. She was awake, alert, responding appropriately with facial expression, mouthing family names in constant eye contact and smiling. Sadly, on 4th August in the afternoon Mrs Alexander deteriorated and died.
- A post mortem was undertaken by Professor Nicholl on 10th August. He reported as follows:
Main Pathological Findings
1. Sagittal sinus thrombosis with extension of thrombus into adjacent superficial cortical veins, the transverse sinuses and sigmoid sinus predominantly on the right side.
2. Extensive venous infarction of the left and right parasagittal regions of the cerebral hemispheres with a large left parietal haematoma (5cm in diameter).
3. Mild brain swelling without internal herniations.
The specific type of damage to the brain, namely venous infarction, which is associated with venous sinus thrombosis is typically associated with haemorrhage in the brain, as found in this case. While it is possible the thrombolysis treatment given may have exacerbated the haemorrhagic component of the infarct, it would also likely have had a tendency to treat the clot in the sagittal sinus itself. However, because there was not significant evidence of severely raised intracranial pressure as a consequence of the hematoma, I think it is more likely that death was due directly to the extensive venous infarction due in turn to the sagittal sinus thrombosis, rather than the intracerebral haemorrhage.
Consequently, I propose as a provisional cause of death:-
1a. Bilateral cerebral haemorrhagic venous infarction
1b cerebral venous sinus thrombosis (thrombolysed)
The evidence of the treating clinicians
Dr Vijay Nar
- As I have explained, Dr Vijay Nar was the registrar on-call for neurology ward cover and referrals on 15th July 2018. He is now a Consultant Neurologist at St Peter's Hospital, Chertsey, Surrey. His witness statement described his examination of Mrs Alexander. He said that when a patient arrives with symptoms of a stroke, "we will always keep in mind important differential diagnoses that can look like a stroke." He included CVST among these, commenting "the possibility of a CVST will always be in the back of my mind." He said:
When a patient arrives with stroke symptoms, speed of treatment is important as 'time is brain ' - as more time passes brain tissue that may be ischaemic can die, worsening the patient's prognosis and increasing morbidity and mortality… The aim is to make a rapid assessment by taking a history and examining the patient, to allow quick investigation and then rapid treatment… [Mrs Alexander's] neurological examination was consistent with a stroke. However, I needed to establish whether it was a haemorrhagic or ischaemic stroke, and thus I organised for her to have a CT head.
- He said that, before Mrs Alexander underwent the scan:
I carried out fundoscopy where I used an ophthalmoscope to examine the appearance of her optic discs. The ophthalmoscope is a standard piece of equipment that a neurologist would carry when examining a patient but is not routinely used during an acute stroke call. I would be looking for signs of raised pressure as a blockage in a vein would lead to increased intracranial pressure which will usually manifest with swollen/ raised optic disc appearances. I would have been trying to get Mrs Runciman into the scanner as soon as possible and I would not normally look at the back of a patient's eyes during a stroke assessment, however, I did do it on this occasion because she had a history of a headache a few days previously. I carried out fundoscopy but did not record it in the notes as we were under time pressure. The results of the fundoscopy were normal.
- He said that a CT Venogram would have taken additional time, as contrast dye would be required and it would be necessary to check Mrs Alexander's kidney function.
I would only consider doing one when I was worried about the potential for the patient having had a cerebral venous sinus thrombosis and an associated venous stroke, as the time delay in an arterial stroke would lead to unnecessary brain tissue loss, but everything in this case was pointing towards an arterial stroke… In my mind the history and presentation were in keeping with an arterial stroke and my top differential diagnosis was that Mrs Runciman had suffered an ischaemic arterial stroke.
- Dr Nar said that he telephoned Dr Morris and they discussed the case and Mrs Alexander's symptoms. Dr Nar's view was that "headache was not one of her primary complaints at presentation". He said that she had one a few days ago but didn't have one now." He said that Dr Morris asked if he had checked for optic disc swelling and he confirmed that there were no signs of raised intracranial pressure. They agreed that Mrs Alexander's presentation was consistent with an arterial stroke and the chance that her presentation was consistent with a venous stroke was low. Dr Morris confirmed that it was appropriate to offer thrombolysis.
- He said that at 12:40 he was called to see Mrs Alexander as she had become agitated and less responsive. He organised a repeat CT head scan which (as set out above) showed biparietal haemorrhage. This did not fit with his initial diagnosis. He now suspected a CVST. A CTV was organised and the diagnosis was confirmed.
- When cross-examined Dr Nar said that headache was not a "primary feature" and had improved. There had been an abrupt onset of focal neurological symptoms, whereas with CVST the onset of symptoms was typically more gradual. He did not agree that headache pointed away from AIS; he agreed that headache could be consistent with CVST, but CVST would be a rare cause. He disagreed that it was necessary to raise "headache" on the "scene guidance" to the radiologists as it was not a big feature at presentation. He said that AIS was his "top differential; there was nothing on the scan to suggest CVST and he would not carry out further investigations unless there was a "viable alternative". It was put to him that it was important to rule out CVST. His response was that no further investigation was necessary unless there was a "viable alternative". He said that there would have been a delay obtaining a CTV. He again emphasised the importance of speedy treatment and that "time is brain".
Assessment of Dr Nar's evidence
- Having looked closely at Dr Nar's notes and his witness statement, and listened carefully to his oral evidence, I am satisfied that he was doing his best to assist the Court. His evidence was substantially supported by his notes and – subject to the specific findings I make below – I accept it.
- There were two apparent discrepancies as between his notes and his oral evidence. The first is as to whether fundoscopy was carried out. This was not recorded in his notes. However, his evidence on this point was supported by Dr Morris (as I explain below) and, since I accept her evidence, I find that he examined the fundi and furthermore, he found no signs of raised intracranial pressure. (I did not understand Ms Lumbers to submit that fundoscopy was not undertaken.)
- The second apparent discrepancy (or lack of clarity) was in relation to the history of headaches. He recorded "4/7 ago frontal HA. Gradual onset. Pressure type." In his witness statement he said that he told Dr Morris that she had "headache in the days prior to onset of symptoms but headache was not one of her primary complaints at presentation. I said that she had had one a few days ago but didn't have one now." In oral evidence he said that he elicited a headache of four days duration, and that it was "verbally handed over to me" that Mrs Alexander had a headache, but she did not have a headache at time of presentation. Dr Morris did not record the details of the discussion relating to headaches in her witness statement but in her oral evidence she said that she was aware of headache "preceding a few days prior." Looking at this overall, I am satisfied that Dr Nar elicited a history of headache, that it did not appear to be a key feature of Mrs Alexander's presentation at the time when he took the history, and I find that Dr Nar discussed this with Dr Morris.
- As I have indicated at [22] an important aspect of his evidence, which was supported by his notes is that he considered CVST at the time. In particular, I find that he discussed this with Dr Morris and with the radiologists before the decision to administer alteplase.
- I find that Dr Nar regarded an acute ischaemic stroke in the middle cerebral artery distribution as the likely diagnosis. This is recorded in his diagnosis and management plan. I find that he therefore concluded that treatment with thrombolysis was indicated and that it was important to administer it as soon as possible.
Dr Rhiannon Morris
- Dr Rhiannon Morris is a Consultant Neurologist at Southampton General Hospital. She was the consultant on-call for acute stroke admissions on the day that Mrs Alexander presented at the hospital. In her witness statement she said that she could not evaluate Mrs Alexander herself as she was dealing with another stroke patient at the time. She said that following Dr Nar's initial assessment of Mrs Alexander she spoke to him by telephone. She was in the department and so she also discussed the case with him in person. They discussed the history and clinical examination and reviewed the CT head scan. She agreed with his opinion that left MCA acute ischaemic stroke was the most likely diagnosis. She asked if there was any papilloedema, and he said that there was no evidence of it. She did consider the possibility of CVST as the potential diagnosis and this was discussed with Dr Nar. On the question of headache she said that it could be a symptom in acute ischaemic stroke as well as CVST, and so it was not sufficient to exclude their working diagnosis. On reviewing the scan, she could not see any obvious features to support a diagnosis of CVST. She contacted the radiology registrar and they were in agreement with her opinion. She said that, based upon the information available at the time, including clinical features, review of the CT scan and radiology opinion, her opinion was that the most likely diagnosis was an acute ischaemic stroke within the left MCA territory. Her decision to give alteplase was based on that information. She said the treatment for AIS is time dependent, with the best outcomes in those patients who are treated soonest after onset of symptoms.
- In her oral evidence Dr Morris said that she could not recall the nuances of the discussion about headaches that she had with Dr Nar, but she was certain that he would have given her the important information about the headache. She confirmed that it was her decision to thrombolyse and that the possibility of CVST was discussed with Dr Nar. She accepted that Mrs Alexander's presentation was consistent with AIS and CVST but the clinical presentation and radiological findings made AIS the most likely working diagnosis. Ultimately, when pressed she said:
You have to make a clinical judgement on the basis of all the evidence. I had the clinical history and examination by Dr Nar and radiological opinion. I would have had to decide that CVST was considerably more likely to AIS to decide it needed to be specifically excluded. This would have led to a delay in administering the treatment I believed to be correct at the time. And the benefit of delivering it - if delayed - would be far less and not lead to an improved outcome. That was the basis for my decision made at that time.
- Dr Morris emphasised that 4.5 hours from the onset of symptoms at 08.30 was the "outer time limit beyond which there would be no obvious benefit of thrombolysis," but that "at 1.5 hours there is a significant improvement compared with three hours." She said there would have been a delay before a CTV could have been obtained and reported. When pressed she said:
In my judgment the time for CTV for a low clinical probability (compared to AIS) would have led to significant delay and the benefit of the correct treatment would have been significantly reduced.
- In her view a description by a patient of a "pressure" headache did not equal intracranial pressure. Furthermore, Mrs Alexander was older than most CVST patients and, with abrupt onset CVST, she would expect to see abnormalities in brain parenchyma in the imaging and that was absent in this case.
- It is convenient to deal at this point with the question of the potential delay which would have arisen from obtaining a CTV. I accept Dr Morris's evidence that there would have been a delay before a CTV could have been carried out and reported. The extent of the delay was not explored in detail in evidence. Dr Nar said that kidney function tests may have been required first. It was pointed out to Dr Morris that when a CTV was obtained at 12:32, it was obtained almost immediately after the second CT scan was reported. But Dr Morris explained that this was because Mrs Alexander was still in the waiting area in the CT department at that time. I note that when the CTV scan was carried out at 12:32, it was not reported until 13.24. The Claimant's own case is that heparin would have been administered "by lunchtime", which clearly implies a delay before the diagnosis was made and after the CTV had been reported. The expert neuroradiologists agreed that a diagnosis of CVST "would have been finalised within an hour of the scan being completed." Taking account of this evidence, I find that the diagnosis would have been made by about 11.30am. I find that this would have been a material delay in the context of the apparent need to administer alteplase urgently.
- The salient point is however that Dr Morris believed that there would have been a delay. I find that the position adopted by Dr Morris on this point was a reasonable one.
Assessment of Dr Morris's evidence
- In my judgment Dr Morris was an impressive witness and the explanation she gave was compelling. I recognise of course that the events in question happened nearly five years ago and she may have gone over them many times. There is always a risk that this may lead a witness to give evidence with greater conviction than is justified. But, having considered her evidence carefully, I thought that Dr Morris gave careful, balanced and thoughtful answers. In particular, she justified her decision to thrombolyse with cogent reasons. She did not seek to fill in gaps in her evidence (for example as to what she knew about the history of headaches); nor did she seek to explain or justify why her account of discussions with Dr Nar differed from his account. She simply gave her account. I have no hesitation in accepting her evidence.
- The evidence of Dr Nar and Dr Morris differed as to whether they spoke in person in addition to by telephone. I think that Dr Morris was probably right on this point, as they were both present in the unit on the day and so I find that they did speak in person as well as speaking on the telephone. I find that they discussed Mrs Alexander's presentation, the likely diagnosis (including the possibility of CVST) and proposed treatment. They must have done so since – as I have indicated - it was a requirement at Southampton that the decision to thrombolyse should be made by a consultant.
- I find that Dr Morris made the decision to offer thrombolysis to Mrs Alexander and that she did so for the reasons she gave in evidence and set out at paragraph 48 above.
Breach of Duty
The allegations
- I turn to consider breach of duty in light of my findings of fact. The Claimant's allegations as set out in the Particulars of Claim are as follows:
a. Failing to appreciate that the Deceased's clinical history was not consistent with arterial ischaemic stroke;
b. failing to recognise that the Deceased's history was consistent with raised intracranial pressure;
c. failing to examine the fundi or vision;
d. failing to provide appropriate clinical information to the radiologist at the CT head at 10:17. This should have included 'raised ICP' instead of '? acute stroke';
e. ruling out SVT on the basis of a plain CT;
f. diagnosing arterial ischaemic stroke;
g. treating with alteplase without first discussing with a senior clinician; the deceased's symptoms and signs were not consistent with acute arterial stroke;
h. failing to refer for the appropriate imaging (CT Venogram) in a timely fashion.
- I can deal straight away with allegations (c) and (g). I have already made findings that the fundi and vision were examined, and that Dr Nar discussed treatment with alteplase with Dr Morris. So those allegations are not made out.
The legal principles
- The legal test for breach was unsurprisingly common ground. It was famously set out by McNair J as a jury direction in Bolam v. Friern Hospital Management Committee [1957] 1 WLR 583 at 587 thus:
…[A surgeon] is not guilty of negligence if he has acted in accordance with a practice accepted as proper by a responsible body of medical men skilled in that particular art… a man is not negligent, if he is acting in accordance with such a practice, merely because there is a body of opinion who would take a contrary view.
- The question in this case therefore is whether no reasonably competent neurologist would have acted and exercised judgment as Dr Nar and/or Dr Morris did.
- In Maynard v West Midlands RHA [1984] 1 WLR 634 at 638, Lord Scarman elucidated the Bolam test thus:
Differences of opinion and practice exist and will always exist in the medical and other professions. There is seldom only one answer exclusive of all others to problems of professional judgement. A court may prefer one body of opinion to the other; but that is no basis for a conclusion of negligence.
- In this case, as in all cases of professional negligence, the parties have adduced expert evidence supporting their positions. But I remind myself that the question as to whether breach has been established is ultimately a matter for the Court, not the experts. I must consider whether the body of opinion relied upon is "responsible, reasonable and respectable" and whether it has "a logical basis": see Bolitho v. City and Hackney HA [1988] AC 232. In this regard, the task of the court is to "see beyond stylistic blemishes and to concentrate upon the pith and substance of the expert opinion and to then evaluate its content against the evidence as a whole and thereby assess its logic.": see C v Cumbria University Hospitals NHS Trust [2014] EWHC 61.
- I approach the expert evidence with all this in mind.
The expert neurologist/ stroke physician evidence
Dr Alakendu Sekhar
- On questions of breach and causation the Claimant relied on the evidence of Dr Alakendu Sekhar. He is a consultant neurologist employed for the last seven years at the Walton Centre NHS Foundation Trust. He is the trust's lead stroke neurologist, and heavily involved in stroke management including thrombolysis. Dr Sekhar also works as a visiting stroke neurologist at Aintree University NHS Foundation Trust and Countess of Chester NHS Foundation Trust. His day-to-day work involves direct clinical care for all aspects of vascular neurology including stroke. He is a member of the Stroke Advisory Group for the Association of British Neurology. I have considered his report on breach of duty and causation dated 17th September 2023, and his additional letters of 11th March 2024 and 21st April 2024.
Dr Christopher Durkin
- On breach and causation, the Defendant relied on the evidence of Dr Christopher Durkin, a consultant stroke physician. He retired from NHS practice at the end of December 2022. For two years before that he worked as an NHS consultant stroke physician at Wycombe Hospital Buckinghamshire. From 1984 to December 2020 he was a full time NHS consultant physician in geriatric and general medicine working at both Stoke Mandeville and Wycombe Hospitals Buckinghamshire Healthcare NHS Trust. He says that he has a special interest in transient ischaemic attack (TIA) and stroke, and that he provided specialist care to stroke patients from 1993 until his retirement. He has 12 years' experience in stroke thrombolysis. I have considered his report on breach of duty and causation dated July 2023. I have also considered his second report on condition, prognosis and life expectancy dated January 2024.
- Whilst Dr Durkin is a stroke physician and Dr Sekhar a neurologist, no point was taken by either side on this. Reference was made at the trial to the "expert neurologists" as a convenient shorthand, and I shall do the same. I am entirely satisfied that both experts were suitably qualified and experienced to give expert evidence on breach and causation.
Dr Sekhar's opinion on breach
- Dr Sekhar's opinion before cross-examination was that Mrs Alexander's presentation should have alerted the treating clinicians to the possibility of CVST. He emphasised her headache and vomiting which could be symptoms of raised intracranial pressure, and he also emphasised the "fluctuating" presentation. His view was that Mrs Alexander's symptoms and signs were not consistent with AIS, that CVST could not be "ruled out" on the basis of a plain CT scan, and that it would be negligent to do so. He considered that the history of headaches and possible raised intracranial pressure should have been included on the CT request form and this would have been valuable "scene guidance".
- Dr Sekhar made important concessions in cross-examination. He agreed that the 4.5 hour limit for the administration of thrombolysis was because infarction would be irreversible thereafter. He agreed that a reasonable body of opinion would regard AIS as the most likely diagnosis in light of the acute onset of focal symptoms and the rarity of CVST. He agreed that a reasonable body of opinion would regard headache as consistent with AIS. He accepted that if the clinicians spoke to the radiologists, then that would be an answer to the allegation about "scene guidance". He also accepted that a patient with AIS could be treated with thrombolysis "with caution".
Dr Durkin's opinion on breach
- Dr Durkin noted the comparative rarity of CVST. He noted that headache was a symptom in many cases of arterial stroke. He noted also the urgency of treatment with thrombolysis as "time is brain". He drew attention to the fact that the time to thrombolysis treatment ("door to needle") is the subject of national audit and monitoring in the Sentinel Stroke National Audit Programme. The national median time to treatment in July 2018 was 50 minutes, and about 55 minutes at Southampton. (In this case I find that it was 43 minutes: see [25] above.) Dr Durkin noted the National Clinical Guideline for Stroke from the Royal College of Physicians which recommended treatment with alteplase for suitable AIS patients within three hours of known onset (which I find would be by 11.30 in Mrs Alexander's case) and that it could be administered at up to 4.5 hours.
- Dr Durkin noted that CVST appeared to have been considered by the treating clinicians and concluded:
Overall and in my opinion the admitting doctors were right to be concerned about acute ischaemic (arterial) stroke and to pursue urgent treatment appropriate to this condition. In my opinion a reasonable body of stroke physicians would have made the same decision at that time and with the information available.
- In cross-examination he emphasised the rarity of CVST and that it was "extremely rare" over the age of 59. He said the treating clinicians would be "failing in their duty" not to give thrombolysis at that time. He rejected the argument that CVST should be "excluded". He thought that it should be considered and investigated with a scan, and given the "time critical" situation the doctors proceeded with thrombolysis "in my view correctly".
Assessment of the experts
- In my judgment, Dr Durkin undertook a comprehensive analysis of this case. He produced a detailed report which analysed all the relevant notes up to and including the post mortem. He extracted relevant clinical guidelines. In his report and when giving evidence he clearly had the Bolam test in mind. When considering breach and causation he analysed and relied upon relevant literature. My assessment is that when giving evidence he gave balanced and measured answers.
72. Dr Sekhar summarised most of the notes in his report, but it is not clear to me that he had Dr Nar's notes clearly in mind since he said that "it is unclear from records whether the history of headaches was captured by the treating physician Dr Nar as clinical notes were sparse…". It is in fact clear that Dr Nar was aware of the history of headache and his notes record this. (This was not explored in evidence. It may be that Dr Sekhar misinterpreted Dr Nar's notes as the stroke nurse's notes.) Dr Sekhar did not refer to the post mortem, despite its obvious importance on questions of causation. He accepted in cross-examination that a "fair analysis" would have included reference to the post mortem. He referred at one point in his report (paragraph 7.2.5) to "any reasonable body of stroke physicians" but, when reading his report and listening to his answers, I formed the clear view that he did not always carefully evaluate the judgments of the treating clinicians against that standard. There was also little recognition in his report of the time pressure, or the need to administer thrombolysis quickly in a suitable case. When giving evidence Dr Sekhar was not an entirely satisfactory witness. He did not always answer questions directly or in a helpful manner. The result was that Mr Barnes had to repeat the same question or ask the question in different ways until it was addressed (for example as to whether acute onset at 08.30 was more consistent with AIS than CVST).
- The result of all this is that I approach Dr Sekhar's evidence with caution. Where his evidence conflicts with that of Dr Durkin, I prefer the evidence of Dr Durkin, but always bearing in mind that it needs to be logical and that I have to "concentrate upon the pith and substance" of the evidence.
Breach - analysis
- Mr Barnes submitted that I should approach the issues with two notes of caution in mind. First, the entire sequence of events – from arrival at the hospital to thrombolysis – occurred within 45 minutes. Second, in cases of this type, it is always important to guard against hindsight; instead we should "put ourselves in the emergency room at 10am." I accept those points.
- At the outset I remind myself of Dr Morris's answers at [48] and [49] above. In my judgment (subject to the point about "scene guidance" which I deal with below) they provide a complete answer to the Claimant's case on breach. Dr Morris had to make a professional judgment. The evidence shows and I find that CVST is rare – accounting for about 0.5% of all strokes. Mrs Alexander was older than a typical CVST patient. She complained of headache, but headache can be a presenting complaint in arterial stroke. There was no evidence of intracranial pressure; fundoscopy was normal; the plain CT scan was normal. The possibility of CVST was discussed with Dr Nar and with the radiologists. Thrombolysis is the accepted treatment for arterial stroke. Importantly it has to be administered quickly, and any delay is likely to lead to a worse outcome.
- Ms Lumbers emphasised that (a) the potential delay in obtaining a CTV may not have been very long, and (b) that alteplase could have been potentially harmful to a patient with CVST. She submitted that these factors should have been weighed in the balance and so CVST should have been ruled out first with a CTV. As to the question of delay, I have found that a diagnosis of CVST would have been made by 11.30am, which would be three hours post the onset of focal symptoms. As for the potentially harmful effect of alteplase, I am satisfied that Dr Morris was fully aware of the potential consequences of administering alteplase and, in any event, Dr Sekhar's evidence did not really support this submission as he thought that alteplase could have been administered "with caution".
- In my judgment Dr Morris's evidence demonstrates that she weighed the material before her, balanced the risks, applied her professional expertise, and reached a judgment in an urgent situation. When listening to the Claimant's case and Dr Sekhar's evidence, I was left with the overriding impression that it depended on hindsight and failed to give sufficient weight to the information that was available to Dr Nar and Dr Morris at the time and to the urgency of the situation.
- Dr Durkin expressed his overall view thus: "In my opinion a reasonable body of stroke physicians would have made the same decision as Dr Morris at that time and with the information available." Standing back and looking at the evidence overall, I am satisfied that Dr Durkin's conclusion is robust, logical and evidence based. I accept it. It follows therefore that, subject to the point on scene guidance which I address below, I find that there was no breach of duty in this case. For completeness, however, I address each of the allegations as set out in the Particulars of Claim.
(a) Failing to appreciate that the Deceased's clinical history was not consistent with arterial ischemic stroke;
- Ms Lumbers submitted that a consideration of the entirety of Mrs Alexander's presentation should have led to an alternative diagnosis being considered. She emphasised the headache, the fact that it was gradual in onset and described as a "pressure" type. She referred also to the evidence of vomiting and nausea, right sided weakness and the "fluctuation" of the focal neurological features.
- Dr Durkin noted that Mrs Alexander presented with a clinical stroke syndrome in that she had abrupt onset of right sided weakness and speech difficulty. She was obese and taking hormone replacement therapy, both of which are risk factors for arterial stroke. Headache is reported in arterial stroke: see A Multivariate Study of Headache Associated with Ischemic Stroke, Ferro et al, Journal of Head and Face Pain, 1995 which found that 34% of ischaemic stroke patients complained of headache. His view was that "the admitting doctors were right to be concerned about acute ischaemic stroke and to proceed with urgent, time critical treatment." I accept this evidence and reject the allegation.
- Dr Sekhar pointed to the development of focal neurological deficits after the onset of a headache which worsened and to vomiting. He said that this would point to raised intracranial pressure (and hence to a diagnosis of CVST). In cross-examination, however, Dr Sekhar confirmed that a reasonable body of neurologists would have concluded that the sudden onset of a focal neurological deficit would make an ischaemic arterial stroke more likely than CVST. He also agreed that, leaving other symptoms aside, having regard to the rarity of CVST, a sudden onset of a focal neurological deficit would make an ischaemic arterial stroke "very likely." He placed some emphasis on what he described as the "fluctuating" nature of Mrs Alexander's presentation. However he accepted that fluctuation did not make CVST more likely, and Dr Durkin strongly disagreed that fluctuation made CVST more likely. Dr Sekhar also agreed that a reasonable body of neurologists would conclude that headache was consistent with AIS. Ultimately he accepted that in light of the scan result and the presentation, Dr Morris's view that this was more likely to be AIS would be consistent with the view of a reasonable body of neurologists.
- I find that Mrs Alexander's presentation was consistent with arterial ischaemic stroke. I find that there was no breach of duty in concluding that the likely diagnosis was arterial ischaemic stroke.
(b) Failing to recognise that the Deceased's history was consistent with raised intracranial pressure;
- Dr Durkin noted that Mrs Alexander suffered from headache, but headache is well reported in AIS, and in the absence of raised intracranial pressure. His view was that Mrs Alexander did not have other features suggestive of raised intracranial pressure, for example visual disturbance or altered consciousness. I accept this evidence. I note also that I have found that fundoscopy was normal and hence there was no evidence of papilloedema. In my judgment, there was in fact no evidence of raised intracranial pressure. I accept Dr Durkin's conclusion was that a reasonable body of stroke physicians would not have diagnosed raised intracranial pressure at that time and with the information available.
(c) Failing to examine the fundi or vision;
- I have already rejected this allegation on the facts.
(d) Failing to provide appropriate clinical information to the radiologist at the CT head at 10:17. This should have included 'raised ICP' instead of '? acute stroke';
- Since there was no negligent failure to recognise that Mrs Alexander's history was consistent with raised intracranial pressure, I reject this allegation. In any event, I have found as a fact that Dr Nar and Dr Morris discussed Mrs Alexander's presentation with the radiologists and that the discussion included a potential diagnosis of CVST. In cross-examination, Dr Sekhar accepted that if there had been such a discussion, this would be an answer to any complaint about lack of "scene guidance" to the radiologists.
(e) Ruling out SVT on the basis of a plain CT;
- It was common ground in the expert joint statement that CVST cannot be ruled out on the basis of a plain CT. Dr Sekhar said in his report: "If it was the clinician's decision to exclude CVST on the basis of plain CT brain this is clearly outside the professional boundaries." Ms Lumbers submitted that Dr Nar's note "no hyperdensity to suggest VST" suggests that CVST was "ruled out" on the basis of the plain CT. In my judgment this misstates the thought process of the treating clinicians; they did not "rule out" CVST on the basis of the plain CT. Their approach was more nuanced. They (in my judgment reasonably) considered arterial stroke to be much more likely and wished to ensure that the appropriate treatment was administered without delay. As Dr Morris put it when cross-examined on her conversation with the radiology registrar:
I would have asked not whether they agreed with my findings, I would have asked the question on whether there were any radiological features that are highly suggestive of a CVST being a more likely diagnosis than arterial stroke. I was not asking them to exclude CVST on the basis of a plain CT.
- Dr Durkin's opinion on this allegation was as follows:
In my opinion the plain CT brain scan was performed to rule out haemorrhage as a prelude to thrombolysis. In my opinion it was not used to rule out cerebral venous sinus thrombosis. In her sworn witness statement, Dr Morris refers to her review of the CT brain scan where she did not see any obvious features to support a diagnosis of CVST… If this evidence is accepted by the court then in my opinion Dr Morris's actions were reasonable.
- In cross examination he confirmed that, given the "time critical" situation, the clinicians proceeded with thrombolysis "in my view correctly", and "their actions were correct and appropriate." I accept Dr Durkin's evidence and I reject this allegation.
(f) Diagnosing arterial ischaemic stroke;
- This adds nothing to the allegation at (a) and I reject it.
(g) Treating with alteplase without first discussing with a senior clinician; the deceased's symptoms and signs were not consistent with acute arterial stroke;
- I have already rejected this allegation on the facts. I find that the decision to administer alteplase was made by Dr Morris. I have also already addressed the question as to whether the symptoms and signs were consistent with AIS; in my judgment, they were. In any event, Dr Sekhar ultimately did not support this allegation. His view in cross examination was that, even if the balance as between AIS and CVST was 50/50 or that CVST was slightly more likely than AIS, it would still have been reasonable to thrombolyse if that was done "with caution". He clarified this to mean that consent should be obtained and the patient monitored.
(h) Failing to refer for the appropriate imaging (CT Venogram) in a timely fashion.
- In closing Ms Lumbers relied on the Ferro paper which states:
In patients with clinically suspected CVT (eg presenting with new headache, isolated intracranial hypertension syndrome, focal neurologic deficits, seizures, and or encephalopathy) urgent neuroimaging is necessary is the first step in the diagnostic evaluation.
- I remind myself of Dr Morris's evidence at [49] above and my finding that it was reasonable for her to conclude that referral for a CTV would have led to a delay which would have been a material delay. Dr Durkin's opinion on this point is as follows:
According to her sworn witness statement, Dr Morris did consider the possibility of CVST and discussed this with Dr Nar. She did not find definite evidence to support a diagnosis of CVST being more likely than the diagnosis of acute ischaemic stroke. In that situation there was in my opinion no definite indication for a CT venogram. In my opinion a reasonable body of stroke physicians would not have arranged a CT venogram on admission. A CT venogram was then appropriately arranged when further brain imaging suggested cerebral venous sinus thrombosis and this examination confirmed the diagnosis.
- In my view, the judgment of Dr Morris, supported by Dr Durkin is logical, coherent and sound. I accept this evidence and reject the allegation.
Conclusion on Breach
- It follows therefore that I reject all the allegations of breach of duty and this claim will be dismissed.
Causation
The Claimant's pleaded case
- The Claimant's case as set out in the Particulars of Claim is as follows:
36. The use of intravenous alteplase on a background of already raised intracranial pressure caused or materially contributed to the multi focal bleeding. The unusual pattern of large haemorrhages seen on the imaging is likely caused by the erroneous administration of alteplase.
37. The propagation of thrombus within the sagittal sinus continued relentlessly in the meantime which contributed to the raised pressure further. The late decision for anticoagulation led to failure of the recanalization of the thrombus, given its extent and spread by this time, and its administration contributed to the extension of the bleed further.
38. A CT venogram would have led to SVT being diagnosed and treated in a timely fashion. The appropriate treatment would have been administration of intravenous heparin, which would likely have been instituted by lunchtime on 15 July 2018. The heparin would have reached the clot, which was only partially occlusive as is apparent on the CTV undertaken at 12.43. With the appropriate treatment the Deceased's death would have been avoided, her life expectancy would have been un-impaired, and recovery would have been complete, on the balance of probabilities.
The legal principles
- The legal principles to be applied were common ground. Both parties relied on Bailey v Ministry of Defence [2009] 1 WLR 1052 at [46] (per Waller LJ):
In my view 1 cannot draw a distinction between medical negligence cases and others. I would summarise the position in relation to cumulative cause cases as follows. If the evidence demonstrates on a balance of probabilities that the injury would have occurred as a result of the non-tortious cause or causes in any event, the Claimant will have failed to establish that the tortious cause contributed. Hotson's case exemplifies such a situation. If the evidence demonstrates that "but for" the contribution of the tortious cause the injury would probably not have occurred, the claimant will (obviously) have discharged the burden. In a case where medical science cannot establish the probability that "but for" an act of negligence the injury would not have happened but can establish that the contribution of the negligent cause was more than negligible, the "but for" test is modified, and the claimant will succeed.
- There was no dispute that:
a. Waller LJ's reasoning on material contribution applies to divisible and non-divisible injuries: Holmes v Poeton Holdings Limited [2023] EWCA Civ 1377;
b. A material increase in risk is insufficient to establish causation in a clinical negligence claim: Gregg v Scott [2005] 2 AC 176, although causation may be established on a balance of probability if the claimant proves that the breach of duty more than doubled the risk of injury: Sienkiewicz v Grief (UK) Ltd [2011] UKSC 10.
Factual causation
- I have concluded at [51] above that there would have been a delay before a CTV was organised and reported. It was common ground that the appropriate treatment would have been low molecular weight heparin (LMWH), and I find that heparin would have been started promptly, that is by 12 noon. I find that alteplase would not have been given.
- There was an issue on the pleadings and between the expert neuroradiologists as to what would have happened if "raised ICP" (intracranial pressure) had been included on the original CT request form. (I have already rejected on the facts the allegation that such a notification should have been included and so there was no breach of duty in this respect.) For the Defendant, Dr Halpin thought that this would not have produced a different CT report. For the Claimant, Dr McConachie thought that reference to ICP would have triggered a closer search for CVST and led to a CTV being performed. On this point I prefer the evidence of Dr Halpin. This is because the signs of CVST on the CT scan were very faint (such that Dr McConachie accepted that a reasonable body of neuroradiologists would not have spotted them) and also because the request for a CTV would have required an assessment of the overall clinical picture which – for reasons which I have explained – did not otherwise indicate CVST.
"But for" causation
- Although Ms Lumbers advanced a case based upon material contribution (and I address this below at [137]), the Claimant's primary position was that this was a case which could be determined on a "but for" basis, ie applying Waller LJ's second proposition in Bailey. The Claimant's pleaded case (as set out at [95]) advanced a case on causation on a "but for" basis, and that is also the way that Dr Sekhar approached the case (see [114] below). The Defendant's position was that the Mrs Alexander would have died in any event, whether or not there was a breach of duty, and so the Defendant relied upon Waller LJ's first proposition.
- The central question is therefore whether on the balance of probabilities Mrs Alexander would have survived, but for the breach of duty. This gives rise to two further questions, namely: (a) what was the effect of giving alteplase? And (b) what would have been the effect of giving heparin?
- There is a key factual question that I must address first before returning to these questions, and that is the extent of the thrombus. This requires an assessment of the imaging.
The expert neuroradiologists
- When interpreting the scans, I have been greatly assisted by the expert evidence of the parties' neuroradiologists. The Claimant called Dr Norman McConachie, a consultant neuroradiologist at Nottingham University Hospitals NHS Trust. The Defendant called Dr Shawn Halpin a consultant neuroradiologist at University Hospital of Wales in Cardiff. I am quite satisfied that both were appropriately qualified to address the issues, and I am further satisfied that both experts were doing their best to assist the Court on the matters within their expertise.
- I have considered the reports of Dr McConachie dated September 2023 and April 2024, together with those of Dr Halpin dated July 2023 and 29th April 2024. The experts also produced two helpful joint statements dated 26th March 2024 and 30th April 2024 (the second one agreed during the course of the trial). Some of the images were shown in Court in the course of the evidence. In the end, as I explain below, there was very little between the experts.
The extent of the thrombus
- I have described the scan reports at [20]-[33] above. Before considering further what they show it is important to bear in mind the limitations of interpretation of imaging, even in the most skilled hands. Dr Halpin explained that in a CTV, contrast medium is injected to opacify the veins. Contrast medium must follow a path from an arm vein to the venous sinuses. CTV data acquisition is a one second snapshot calculated to coincide with the arrival of contrast medium into the venous sinuses. Dr Halpin said that typically 20 to 30 seconds passes from injection into the arm vein until the cerebral venous sinuses are maximally opacified, but sometimes opacification is delayed. He did not think it possible to determine from a one second snapshot whether or not there was complete or incomplete occlusion.
- There are three CTVs to consider. The first was reported at 13:24 on 15th July, the day of admission. The relevant extract is set out at [29] above. It described a "long segment filling defect within the superior sagittal sinus." Dr McConachie's original view was that there was "non-occlusive thrombus throughout the superior sagittal sinus" with a small volume of thrombus also evident in the lateral left transverse sinus and upper jugular vein." In his second report, Dr Halpin commented:
In my opinion, from the extent of the thrombus on the plain scan and the CTV, and from the marked degree of distension of cerebral veins that are trying to drain into the sagittal sinus, there is a lengthy venous sinus thrombosis, running the whole length of the superior sagittal sinus on all scans from 15.7.18 and this thrombosis is having a significant hemodynamic effect on cerebral venous drainage and hence cerebral perfusion; and that pressure inside the cerebral veins would have been abnormally high.
- In the second Joint Statement Dr Halpin commented that there was a heavy thrombus load causing a severe haemodynamic constraint on venous flow such that the degree of occlusion, while being less than 100%, is highly significant. When it was put to him, Dr McConachie agreed that the constraint on haemodynamic flow and the degree of occlusion were "highly significant".
- The second CTV was undertaken two days later on 19th July. The report is extracted at [32] above. The report commented that that there was probably not extension but maturation of the clot. Surprisingly, Dr McConachie missed the fact that a CTV had been undertaken at the same time as the CT scan and did not refer to it at all in his report. He accepted that this was an error. In his first report Dr Halpin said that "the extensive thrombus has not significantly changed." The first Joint Statement did not refer to this scan. In the second Joint Statement the experts noted:
We agree that there is less contrast opacification within the sinus than on the previous CTV. Thrombus has also propagated (extended). Dr Halpin considers that this may be at least in part due to technical factors and timing, but we agree that the appearance has deteriorated in the four days interval. We agreed that this would further impair penetration of the thrombus by heparin.
- The third CTV was five days later on 24th July. Mrs Alexander had not improved. The scans were sought to "check for evidence of recannulation", heparin having been administered from 19th July. The report is at [33] above. This noted "maturation" of the thrombus and "no evidence of recanalization". In their first joint statement the experts agreed that this showed "progression of the thrombosis". In his first report Dr McConachie said that "thrombus now largely fills the superior sagittal sinus and torcular and there is progressive non occlusive thrombosis of the left transverse/ sigmoid sinuses and jugular vein". Dr Halpin's view in his report was that the CTV "showed no significant change". Dr McConachie's view in his second report was that at this point the amount of contrast penetrating the superior sagittal sinus had increased again compared to 19 July 2018, although it had not recovered to the baseline level seen on 15 July 2018. There was slightly more thrombus in the left transverse sinus and jugular vein but it remained partly occlusive. There was also more thrombus in the straight sinus (which drains blood from the deep parts of the brain) with evidence of engorged collateral venous drainage pathways having developed."
- The final relevant report is the post mortem; see the report at [35] above.
- Finally on this part of the case I note Dr Durkin's opinion. Whilst he deferred to the neuroradiologists on interpretation of the imaging, he noted that he had experience of thousands of scans, including those showing CVST. In his view there was "no definite evidence of either propagation or resolution."
Conclusion on the extent of the thrombus
- Looking at the evidence overall, I find that there was at all times a lengthy venous sinus thrombosis running the entire length of the sagittal sinus with some thrombus extending in to adjacent veins. The experts agreed and I accept that on 15th July at the time of admission there was already a heavy thrombus load which had a highly significant haemodynamic constraint, and the degree of occlusion was highly significant. Whilst there was agreement that the thrombus had "extended" on 19th July, I find that any extension must have been marginal. This is because Dr Halpin's original view was that it had not significantly changed and because the report referred to maturation, not extension. (It is to be borne in mind that this scan was taken four days after the administration of alteplase which would have had a tendency to treat the clot.)
- The scan on 24th July was taken after heparin had been administered for five days. The experts agreed that the thrombus had progressed. But I note the original report that referred to "maturation" and Dr Halpin's original view that there was no significant change. I find that any progression was marginal. I find that that there was no evidence of recanalization.
The expert opinions on causation
Dr Sekhar's opinion
- Dr Sekhar's initial analysis of causation was set out in five paragraphs at the end of his report. He concluded:
10.1. But for the failure to diagnose the deceased with cerebral venous sinus thrombosis and provide early administration of the appropriate treatment for cerebral venous sinus thrombosis, the extent of the brain damage caused by the swelling of the brain and repeated haemorrhages would have been avoided, hence the reduction of the extent of the permanent brain damage and death caused.
10.2 Haemorrhage is a well documented and frequent result of venous infarction following venous sinus thrombosis; however, the deceased's admission CT was devoid of established venous infarction or any signs of haemorrhage. I am of the view that but for the administration of intravenous thrombolysis the deceased would have survived and, at worst, lived with some degree of disability.
10.3 Similarly, if appropriate administration of intravenous heparin instituted by lunchtime on 15th July 2018, the heparin would have reached the clot, the burden was only partially occlusive the deceased death would have been avoided and at worst would have lived with some degree of disability.
…
10.5… she was treated for arterial ischemic stroke and the use of thrombolytic drugs exacerbated the bleeding in presence of the brain swelling which has been already ensued due to increased venous congestion secondary to raised pressures in the partially occluded sigmoid and transverse sinuses.
…
10.7 It is arguable whether the haemorrhage could be entirely prevented and on the balance of probability at least the extent of haemorrhage could have been lessened by early administration of the heparin and consideration of neuro interventional strategy such as direct injection of alteplase via micro catheter navigated into the thrombosed sinuses. [This last point was not pursued at trial. The Claimant's case was that the appropriate treatment was heparin.]
[sic]
Dr Durkin's opinion
- In his report, Dr Durkin first considered the cause of the intracerebral haemorrhage. His opinion was that it had a number of possible causes and the most likely of these was venous infarction due to venous sinus thrombosis. He pointed in particular to the later brain scan findings of venous infarction and the post mortem findings. He noted however that haemorrhage is a well-recognised consequence of thrombolysis for ischaemic stroke. He reviewed a paper Risk of intracerebral hemorrhage with alter players after acute ischaemic stroke, Whiteley et al, Lancet Neurology 2016, 15. He concluded that the considerable majority of patients treated with alteplase (for ischaemic stroke) did not suffer an intracerebral haemorrhage. His conclusion therefore was that on balance the extent of the venous sinus thrombosis and resulting venous infarction would have resulted in haemorrhage in any event. He conceded however that there is a "valid debate" about whether the administration of thrombolysis increased the amount of haemorrhage produced by the existing venous infarction and therefore made a material contribution to that haemorrhage. He commented that the absence of infarction on an early scan was not unusual "as the appearances of infarction may not appear for a number of hours after vessel occlusion." In his opinion as a stroke physician "the pattern of haemorrhages is suggestive of hemorrhagic venous infarction."
- Dr Durkin next considered the effect of heparin. He noted that anticoagulation with heparin is the treatment recommended by the UK and European guidelines for CVST, but in his view the evidence base for this treatment is surprisingly weak. It amounts essentially to two small randomised clinical trials involving only 79 patients. His conclusion was that it is not possible to use the figures from the review in support of the treatment effect in this case. He further relied on a paper by Montalvan et al to the effect that Mrs Alexander was in a group with a poor prognosis even with anticoagulation. In evidence he made the point that "heparin was given and there was no effect on the thrombus during that period."
- His conclusion was that "on the balance of probabilities the outcome would not have been significantly different even with earlier treatment with heparin." He reviewed the post mortem findings and concluded on the balance of probabilities that the administration of thrombolysis did not cause Mrs Alexander's death, notwithstanding the development of intracerebral haemorrhage.
Joint statement
- There was no agreement on causation in the Joint Statement. Dr Durkin – as set out above – noted Dr Halpin's opinion on the extent of the thrombus and that there was no definite evidence of either propagation or resolution. He repeated that a "normal" CT scan does not exclude venous infarction. In his opinion heparin would not have removed the extensive thrombosis and death would not have been avoided on the balance of probabilities. He referred once again to the post mortem findings which in his view suggested "that death resulting from extensive bilateral venous infarction would not have been avoided even if there was less intracerebral haemorrhage."
- Dr Sekhar's view was that the radiological changes seen in the initial CTV were "fairly mild" and heparin would have "reduced the propagation of the thrombus". On balance, he concluded death was precipitated by "intracranial haemorrhage contributed by oozing distended cortical veins and precipitated by the potent immediate effects of alteplase administration." He concluded that the post-mortem findings of venous infarction were a late phenomenon and were absent before the administration of alteplase and so were not the "sole cause" of death. In cross examination he hesitated before finally saying that – with alternative treatment - death would have been avoided on balance of probabilities.
The parties' submissions
- For the Claimant, Ms Lumbers submitted that (a) the literature shows that Mrs Alexander's prognosis was good prior to the administration of alteplase; (b) studies show that heparin is likely to be efficacious; (c) heparin would have been effective to prevent the propagation of the thrombus; (d) Mrs Alexander would have suffered "some small degree of haemorrhage"; (e) the extent of the haemorrhage was increased by the administration of alteplase; (f) death was caused or contributed to by the failure to give heparin which led to the propagation of the thrombus and also by the large bilateral haemorrhages. She relied upon the opinion of Dr Sekhar.
- For the Defendant, Mr Barnes submitted that the evidence demonstrated that (a) haemorrhage is likely to have occurred in any event; (b) thrombolysis did not cause additional bleeding; (c) in any event infarction, not haemorrhage, was the cause of death; (e) heparin would not have reduced the extent of the infarction so as to avoid death, and so (f) Mrs Alexander would have died anyway even if she had been treated with heparin and not with alteplase.
Causation - analysis
The experts
- I have already noted my misgivings about Dr Sekhar's evidence when considering breach. On the question of causation I prefer the evidence of Dr Durkin by a significant margin. In my judgment his approach was rigorous, logical and evidence based. Importantly in my view, his opinion was consistent with the post mortem findings and was informed by a review of relevant literature. I have already mentioned that Dr Sekhar did not refer to the post mortem. His view that "death was precipitated by intracranial haemorrage contributed by oozing distended cortical veins and precipitated by the potent immediate effects of alteplase" was absent from his report and first raised in the Joint Statement. Furthermore, he proceeded on the basis that the radiological changes in the first CTV were "fairly mild". If he intended to convey the view that the extent of the thrombus was fairly mild at that stage, then I reject it for the reasons set out above. In my judgment, in reaching his opinion on causation, Dr Sekhar failed to give sufficient weight to the extent of the thrombus in the period 15th to 24th July and he failed to give any weight at all to the findings at post mortem. I do not regard his opinion as a secure base from which to approach the issues of causation.
The academic papers
- Ms Lumbers relied on academic papers in support of her submission that Mrs Alexander's prognosis would have been good on admission. She took the Court first to the International Study on Cerebral Vein and Dural Sinus Thrombosis (Ferro et al, 2004) which studied 624 patients. She submitted that it recorded an 8.3% overall death rate and that Mrs Alexander's prognosis would therefore have been good. She relied next on A Practical Score for Prediction of Outcome after Cerebral Venous Thrombosis, Barboza et al 2018. She submitted that applying the paper's risk prediction score, Mrs Alexander's implied mortality risk was 1.1% at admission.
- She then referred to Predicting Poor Response to Anticoagulation Therapy in Cerebral Venous Thrombosis using a Simple Clinical-Radiological Score, Montalvan et al 2022. She submitted that this showed that Mrs Alexander would have been at low risk for poor outcome of anticoagulation. I do not accept this submission. Dr Durkin's view was that, having regard to the scoring system, Mrs Alexander would have been predicted a poor outcome because there had been a clinical deterioration after admission. There was some debate in evidence as to whether Mrs Alexander had indeed deteriorated after admission. The evidence is that the ambulance notes recorded at handover "remains as described above until arrival and hand over at ED but thereafter does not seem able to speak at all." Dr Nar's notes referred to "mild improvement". But the GCS at 09.17 was 15 and at 10:30 (before the administration of alteplase) it was 14. I find that on the basis of the GCS scores and the ambulance notes that Mrs Alexander would have fallen into the category of those with a poor prognosis on the basis of the Montalvan paper.
- Dr Durkin emphasised and I accept that the scoring systems in the academic papers could not take account of the extent of the thrombus in the present case which was 24-27cm. I also accept his point that the papers "all suffer from the same shortcoming; they are not randomised control studies, they are descriptions of what happened." In my judgment the papers dealing with prognosis are undeniably helpful in setting the context and I accept that the prognosis for CVST is good in a large majority of cases. Nonetheless, it is axiomatic that I must focus primarily on the facts of Mrs Alexander's case.
Infarction
- It is clear that by time of the post mortem there was extensive bilateral infarction (dead tissue). Infarction secondary to CVST was given as the cause of death. Dr Durkin's clear view, which I accept, was that infarction would have followed ischaemia (restricted blood supply) and this process would have been in train from the onset of focal symptoms at 08:30 on 15th July. His view was that early brain scans are often normal. Dr McConachie accepted that ischaemia would have been present at the time of the first scan though not seen on the image. Infarction was not identified on a scan until 19th July. There was not much evidence as to the likely time frame within which ischaemia would have progressed to infarction. Dr Durkin noted that the rate at which that occurs in acute ischaemic stroke is relatively rapid, hence the need for alteplase within 4.5 hours. He thought that gave an "indication" but cautioned that CVST is such a rare condition that it is hard to say. He was however clear that ischaemia would have been present from 08.30 and would have progressed to infarction as was ultimately seen at post mortem. I accept this opinion.
Haemorrhage
- Ms Lumbers accepted and I find that Mrs Alexander would have suffered haemorrhage in any event. Haemorrhage is a well-recognised consequence of CVST. There was a dispute as to whether the administration of alteplase contributed to the extent of the haemorrhage. Dr Durkin noted that haemorrhage was a well-documented consequence of thrombolysis for ischaemic stroke, but drew attention to a paper by Whiteley et al (2016) which noted that a considerable majority of patients treated with alteplase did not suffer haemorrhage. Nonetheless, he accepted that there was a "valid debate" to be had on this point. Dr Halpin and Dr McConachie both thought that alteplase had "promoted or precipitated" haemorrhage, though they deferred to the neurologists on causation. It was accepted that a side effect of alteplase is bleeding. Having regard to the timing of the haemorrhage and the administration of alteplase, I find that alteplase did make the haemorrhage worse and materially contributed to it.
The effect of heparin
- Ms Lumbers relied on papers dealing with the effect of heparin. There is in fact surprisingly little literature on this issue. She noted that in one randomised trial (Einhaupl et al), a trial of 60 patients was stopped early after 20 patients were enrolled because of the apparent benefit of the treatment. Mr Barnes submitted that this should be disregarded as it dealt with patients treated with intravenous high dose unfractionated heparin, so not the same drug as was administered to Mrs Alexander. The second trial (de Bruijn et al) was for 59 patients. I accept that these papers provide some support for the efficacy of heparin but I also accept Dr Durkin's point that the evidence base for the treatment is surprisingly weak.
- Nonetheless, as Dr Durkin accepted, anticoagulation with heparin is the treatment recommended by the UK and European guidelines for CVST. He drew attention to Anticoagulation for Cerebral Venous Sinus Thrombosis ed. Couthino et al, 2011 which reviewed the studies and concluded that although anticoagulant treatment is safe, it is associated with a "reduction in the risk of death or dependency which did not reach statistical significance." I accept this point.
- The evidence shows that heparin works by "bathing" the thrombus. It does not dissolve the thrombus but it prevents propagation and allows the body's own mechanisms to "recanalise" the affected veins. It was agreed by the neuroradiologists that the penetration of the thrombus by heparin would have been impaired on 15th July and further impaired on 19th July. There is no reliable evidence to support the assertion that any additional loss of penetration of the thrombus would have affected the efficacy of the anticoagulant. It was agreed that this was a process that took some time. Dr Sekhar thought that reducing the size of the thrombus would occur "within a week, maybe a few days". Dr Durkin said that "studies suggest weeks and months but even after three months full canalisation was not achieved in most patients." I accept Dr Durkin's view on this point but, even if Dr Sekhar is right as a matter of generality, his view is not supported by the evidence in Mrs Alexander's case since I find that there was no material improvement after five days of treatment with heparin. There was no evidence of recanalization, and the thrombus had marginally progressed.
- Since there were only minimal changes to the thrombus as between 15th and 19th July, and between 19th and 24th July, I find further on balance that there would have been no meaningful improvement in the thrombus even if heparin had been given on 15th July. This means that infarction would have continued to develop.
The cause of death
- I find that the cause of death was as given on the post mortem report, that is infarction secondary to CVST. In coming to his conclusion Prof Nicholl relied in particular on the extent of the thrombus. Dr Durkin expressed the same view and I accept it.
- Whilst I have found that the administration of alteplase contributed to the haemorrhage I find that the haemorrhage did not cause or contribute to Mrs Alexander's death. The post mortem noted the haemorrhage but expressly found that the haemorrhage did not contribute to Mrs Alexander's death. Dr Durkin expressed the same view and I accept it. Indeed it appears that Dr Sekhar ultimately accepted this point since, when asked to consider the post mortem, the following exchange took place:
Q: I think you accept the findings at post mortem, but the point is how that situation arose?
A: Yes
Q: The reality is, insofar as haemorrhage is concerned, it is not the cause of the presentation at post mortem?
A: Because of the post mortem findings?
Q: Yes
A: No
- I find that if heparin had been given on 15th July instead of alteplase, this would not have prevented infarction and hence Mrs Alexander would sadly have died anyway. This was Dr Durkin's view and I accept it. In cross examination he was clear that venous infarction would not have been avoided in any event, even with the earlier administration of heparin. In my judgment his opinion on this point is supported by the extent of the thrombus and the lack of effect of heparin when it was given for five days. It is also supported to some extent by the lack of improvement which followed the administration of alteplase. As Dr Durkin noted, alteplase has been used as a treatment for CVST, although the evidence base for this is small.
Conclusion on "but for" causation
- Drawing these threads together, I find on the balance of probabilities that the extent of the thrombus was at all times extensive; that heparin had no material effect when administered for five days; that alteplase contributed to the haemorrhage; that haemorrhage did not cause or contribute to Mrs Alexanders's death; that her death was caused by infarction secondary to CVST; and that Mrs Alexander would still have died even if CVST had been diagnosed promptly and she had been given heparin, not alteplase, on 15th July.
- I accept Ms Lumbers' point that the literature shows that CVST is a stroke with a good prognosis in a substantial majority of cases, but it is necessary to focus on the facts of this particular case. In my judgment Mrs Alexander fell outside the group of patients with a good prognosis. Notwithstanding the careful submissions of Ms Lumbers, to my mind the Claimant's case failed to give adequate weight to the facts that (a) the thrombus was extensive from the outset, (b) there was no real evidence of any improvement after treatment with heparin for five days, and (c) the cause of death was infarction secondary to CVST.
Material contribution
- For completeness, I will address the Claimant's argument on material contribution. In her written submissions, Ms Lumbers relied on material contribution and Waller LJ's third proposition in Bailey, although the legal argument was not developed further. She submitted that the Claimant would succeed if the administration of alteplase caused at least some bleeding and/or the failure to administer heparin earlier caused at least some propagation of the thrombus. But in reality it seemed to me that the Claimant's case depended upon "but for" causation and the second proposition. That is consistent with paragraph 38 of the Particulars of Claim. I did not understand Ms Lumbers to submit that this is case where medical science could not establish "but for" causation. Indeed the medical evidence advanced by the Claimant addressed that very issue, and the Claimant's case was that, but for the alleged breaches, Mrs Alexander would have survived. That was Dr Sekhar's view. In my judgment, on the basis of my findings of fact, this case falls squarely within the class of cases (for example Hotson v. East Berkshire Health Authority [1987] 1 AC 750) covered by Waller LJ's first proposition. I have found on the facts that, on the balance of probabilities, the alleged breaches (if established) did not cause or contribute to Mrs Alexander's death. She would not have survived, even if there had been no breach of duty.
Overall Conclusion
- I have re-read Mr Runciman's evidence. I am fully conscious that there is a family bereavement at the heart of this case and that the consequences have been devastating for Mr Runciman and his wider family. But, having carefully considered the evidence and the arguments, I conclude that:
a. there was no breach of duty on the part of the Defendant's treating clinicians;
b. if the Claimant had established a breach of duty on the part of the Defendant, such breach of duty did not cause or contribute to Mrs Alexander's death.
- Accordingly the claim is dismissed.
Consequential Matters
- I invite the parties to agree an Order giving effect to this judgment and any consequential matters including costs. This should be done within 7 days of hand-down. If agreement cannot be reached, then the parties should lodge written submissions on any outstanding matters within the same timescale. I will then decide any disputed points on the papers or – if either party requests it – list the matter for a hearing.
- I am grateful to Ms Lumbers, Mr Barnes, their instructing solicitors, and the parties for their assistance.